Diving into the realm of the best diet for Crohn’s disease in 2025, this introduction sets the stage for an insightful journey, providing a comprehensive overview of what lies ahead in the world of dietary management.
Detailing the importance of diet in managing Crohn’s disease and the impact it has on overall health, this introduction aims to captivate readers from the get-go.
Overview of Crohn’s Disease and Dietary Management
Crohn's disease is a chronic inflammatory condition that affects the digestive tract, causing symptoms such as abdominal pain, diarrhea, fatigue, and weight loss. It can impact any part of the digestive system, from the mouth to the anus, and can also lead to complications like ulcers, strictures, and fistulas.Diet plays a crucial role in managing Crohn's disease, as certain foods can trigger inflammation and worsen symptoms, while others can help reduce inflammation and improve overall digestive health.
A well-balanced diet can not only alleviate symptoms but also reduce the risk of flare-ups and complications associated with the disease.
The Role of Diet in Managing Crohn’s Disease
- Eating a low-residue diet: This involves consuming foods that are easily digested and leave minimal residue in the intestines, which can help reduce inflammation and minimize symptoms.
- Avoiding trigger foods: Certain foods, such as dairy, gluten, spicy foods, and high-fiber foods, can trigger inflammation and exacerbate symptoms in individuals with Crohn's disease.
- Increasing intake of anti-inflammatory foods: Foods rich in omega-3 fatty acids, antioxidants, and probiotics can help reduce inflammation and promote gut health, leading to improved symptoms and overall well-being.
- Staying hydrated: Drinking an adequate amount of water is essential for maintaining proper digestion and preventing dehydration, which can worsen symptoms of Crohn's disease.
- Consulting with a dietitian: Working with a registered dietitian can help individuals with Crohn's disease create a personalized and sustainable diet plan that meets their nutritional needs and supports their digestive health.
Current Dietary Recommendations for Crohn’s Disease
Crohn's disease is a chronic inflammatory condition that affects the digestive tract, leading to symptoms such as abdominal pain, diarrhea, and fatigue. Proper dietary management plays a crucial role in managing the symptoms and improving the quality of life for individuals with Crohn's disease.
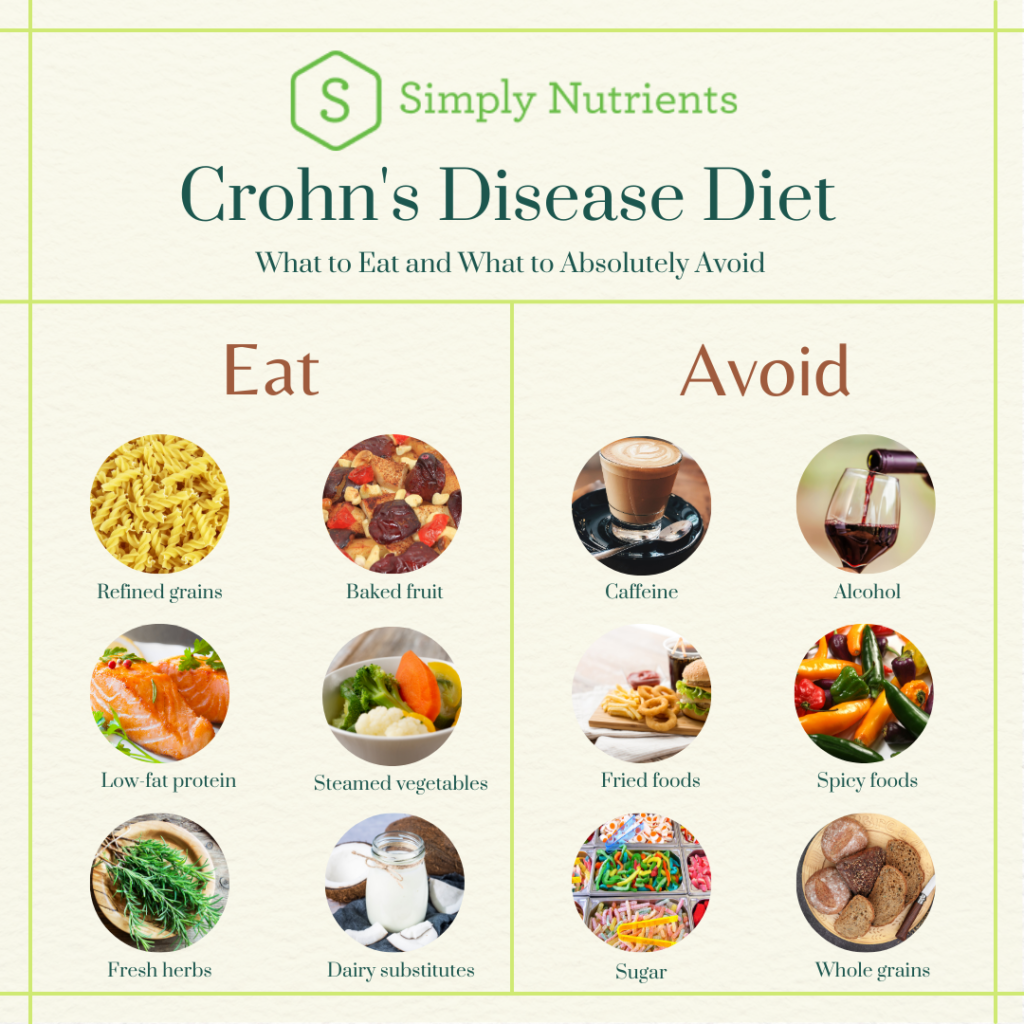
Types of Foods to Include in a Crohn’s-Friendly Diet
- Low-fiber fruits and vegetables: Opt for well-cooked or peeled fruits and vegetables to reduce fiber content, which can be hard to digest.
- Lean proteins: Include sources of lean protein such as poultry, fish, and eggs to support muscle health and overall nutrition.
- White grains and refined carbohydrates: Choose white rice, pasta, and bread over whole grains to ease digestion and minimize irritation to the intestines.
- Dairy alternatives: If lactose intolerant, opt for lactose-free or plant-based alternatives like almond milk or soy yogurt.
- Healthy fats: Incorporate sources of healthy fats like avocado, olive oil, and nuts to support nutrient absorption and reduce inflammation.
Foods to Avoid or Limit to Manage Crohn’s Symptoms Effectively
- High-fiber foods: Limit high-fiber foods like nuts, seeds, and raw fruits and vegetables, as they can exacerbate symptoms like bloating and gas.
- Spicy foods: Avoid spicy foods that can irritate the digestive tract and trigger inflammation in individuals with Crohn's disease.
- Dairy products: Some individuals with Crohn's disease may be sensitive to dairy, so it's important to limit or avoid dairy products that worsen symptoms.
- Caffeine and alcohol: Limit intake of caffeine and alcohol, as they can stimulate the intestines and worsen diarrhea and abdominal discomfort.
- Sugar and artificial sweeteners: Reduce consumption of sugary foods and beverages, as well as artificial sweeteners that can disrupt gut health and aggravate symptoms.
Emerging Trends and Research in Dietary Management
As research in the field of Crohn's disease continues to advance, new trends and innovative approaches in dietary management are constantly being explored. These emerging strategies offer hope for improved quality of life and symptom management for individuals living with this condition.
Personalized Nutrition Plans
One of the exciting trends in dietary management for Crohn's disease is the shift towards personalized nutrition plans. By tailoring diet recommendations to individual needs and preferences, patients may experience better symptom control and overall well-being. This approach takes into account factors such as food sensitivities, nutrient deficiencies, and gut microbiome composition to create a customized diet that supports optimal health.
Anti-Inflammatory Diets
- Research suggests that anti-inflammatory diets, such as the Mediterranean diet or specific dietary patterns rich in fruits, vegetables, whole grains, and healthy fats, may help reduce inflammation in the gut and alleviate symptoms of Crohn's disease.
- These diets focus on incorporating foods with anti-inflammatory properties, such as omega-3 fatty acids, turmeric, ginger, and green tea, which have been studied for their potential benefits in managing inflammation associated with Crohn's disease.
Nutritional Supplements and Functional Foods
- Recent studies have shown promise in the use of nutritional supplements and functional foods to support gut health and reduce inflammation in patients with Crohn's disease.
- Probiotics, prebiotics, and specific micronutrients like vitamin D and zinc are being investigated for their role in modulating the gut microbiome and improving symptoms of Crohn's disease.
Fasting and Intermittent Fasting
- Emerging research suggests that fasting and intermittent fasting regimens may have potential benefits for individuals with Crohn's disease, such as reducing inflammation, promoting gut healing, and improving overall digestive health.
- By giving the digestive system a break and allowing for periods of rest, fasting approaches could help manage symptoms and optimize nutrient absorption in Crohn's patients.
Personalized Nutrition for Crohn’s Patients
Personalized nutrition plans play a crucial role in managing Crohn's disease as they are tailored to meet the specific needs and symptoms of each individual. These customized dietary recommendations can help alleviate symptoms, reduce inflammation, and improve overall quality of life for patients.
Importance of Personalized Nutrition Plans
Personalized nutrition plans take into account the unique triggers and sensitivities of each individual with Crohn's disease. By identifying specific foods that may aggravate symptoms or cause flare-ups, these tailored plans can help patients make informed decisions about their diet and optimize their nutrition intake.
Developing Personalized Dietary Recommendations
Healthcare professionals, such as dietitians and gastroenterologists, play a key role in developing personalized dietary recommendations for Crohn's patients. By conducting thorough assessments of patients' medical history, symptoms, and nutritional needs, healthcare providers can create individualized plans that address specific concerns and goals.
Role of Healthcare Professionals
Healthcare professionals work closely with Crohn's patients to monitor their progress, adjust their nutrition plans as needed, and provide ongoing support and guidance. By collaborating with a multidisciplinary team, including doctors, nurses, and nutrition experts, patients can receive comprehensive care that addresses all aspects of their health and well-being.
Nutritional Supplements and Their Impact on Crohn’s Disease
Nutritional supplements play a crucial role in addressing common deficiencies in individuals with Crohn's disease and supporting overall health. These supplements can help bridge the gap in essential nutrients that may not be adequately absorbed due to the condition.
Common Nutritional Deficiencies in Crohn’s Patients
- Iron: Deficiency can lead to anemia and fatigue.
- Vitamin B12: Important for nerve function and red blood cell production.
- Vitamin D: Essential for bone health and immune function.
Role of Nutritional Supplements
Nutritional supplements can help individuals with Crohn's disease meet their daily nutrient requirements and prevent deficiencies. They provide a concentrated source of vitamins, minerals, and other essential nutrients that may be lacking in their diet.
Types of Supplements for Crohn’s Patients
- Probiotics: Support gut health and immune function.
- Omega-3 fatty acids: Reduce inflammation and support heart health.
- Calcium: Essential for bone strength and overall health.
Lifestyle Factors and Dietary Considerations
When managing Crohn's disease, it is essential to consider lifestyle factors that can impact symptoms and overall well-being. Factors such as stress, sleep, and exercise play a crucial role in disease management and can complement dietary strategies for better symptom control.
Influence of Stress on Crohn’s Disease
Stress is known to exacerbate Crohn's disease symptoms and trigger flare-ups. High stress levels can weaken the immune system and increase inflammation in the gut, leading to digestive issues. Finding ways to manage stress, such as through relaxation techniques, therapy, or mindfulness practices, can help reduce symptom severity in Crohn's patients.
Importance of Quality Sleep
Adequate sleep is vital for overall health and plays a significant role in managing Crohn's disease. Poor sleep patterns can disrupt the body's immune function and increase inflammation, worsening symptoms in patients with Crohn's. Establishing good sleep hygiene practices, such as maintaining a consistent sleep schedule and creating a relaxing bedtime routine, can improve symptom control and overall well-being.
Benefits of Exercise for Crohn’s Patients
Regular exercise can have numerous benefits for individuals with Crohn's disease. Physical activity helps reduce inflammation, improve digestion, and boost overall mood and energy levels. Incorporating a mix of cardiovascular, strength training, and flexibility exercises into daily routine can support symptom management and enhance quality of life for Crohn's patients.
Last Point
In conclusion, the discussion on the best diet for Crohn’s disease in 2025 sheds light on the evolving landscape of dietary management, offering hope and possibilities for those seeking effective ways to navigate this condition.
Clarifying Questions
What are the common nutritional deficiencies in Crohn’s patients?
Nutritional deficiencies in Crohn’s patients often include vitamin D, vitamin B12, iron, and calcium.
How can personalized nutrition plans benefit individuals with Crohn’s disease?
Personalized nutrition plans can cater to specific needs and symptoms of Crohn’s patients, optimizing their dietary intake for better management of the condition.
What role do lifestyle factors play in Crohn’s disease management?
Lifestyle factors like stress, sleep, and exercise can significantly impact Crohn’s disease management, complementing dietary strategies for enhanced symptom control.